Primary Care Networks (PCNs) support General Practitioners (GPs) connected via a virtual network on their provision of care through a holistic team-based care approach. A PCN is a network of GPs supported by nurses and care coordinators. This team-based care approach ensures patients are better cared for in the community.

The PCN Application Call was launched on 1 April 2017. From 1 January 2018 onwards, successfully awarded PCNs (and their GPs) were able to tap on funding and administrative support to implement team-based care to better monitor and manage their patients’ healthcare needs. The PCN scheme also provides participating GPs with a platform for the cross-sharing of best practices for patient care. to enable the three paradigm shifts needed to sustain our healthcare system beyond 2020 - Beyond Hospital to Community, Beyond Quality to Value, and Beyond Healthcare to Health. To effect these shifts, we need to transform our primary care to ensure that good quality and affordable care is accessible and delivered in a sustainable manner in the community. GPs need to join a PCN to participate in Healthier SG, a major transformation of our healthcare system to promote good health, prevent chronic diseases and their deterioration, anchored by primary care and the community, which was rolled out in July 2023. GPs, like yourself, are located close to your patients’ homes; as a result, you play an instrumental role in the management of our ageing and increasingly complex chronic patient population.
To support your role in providing more holistic chronic disease management for your patients and working closely with them to make lifestyle modifications, funding and administrative support is now available to you under the PCN scheme.
How do PCNs work?
First, the patient consults a PCN GP for his or her chronic condition(s). As a PCN GP, you will assess and diagnose the patient’s condition(s) and work with him/her to co-create his/her health plan. The patient should also be referred to see a nurse counsellor and the relevant ancillary services such as Diabetic Foot Screening or Diabetic Retinal Photography, if necessary.
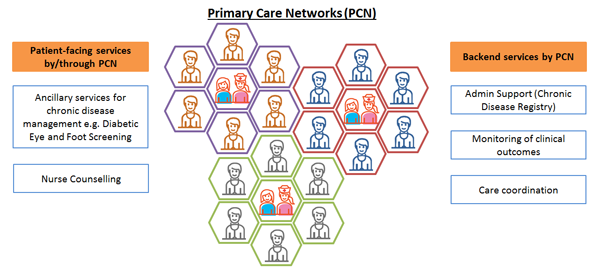
The care coordinator at the PCN-HQ level will then work with the respective clinic assistant to schedule the patient for the ancillary service appointment. Upon completion of the ancillary service(s), the doctor will review the test results and follow up with the patient.
The patient’s progress and clinical outcomes will be tracked and monitored to ensure that they follow through with their personalised care plans and treatment. The overall aim is to help patients better manage their chronic conditions and improve their health outcomes.
For more information on PCN and information on PCN services and support, please click here.

