Goals of management of COPD
a) Relieve symptoms
b) Improve exercise tolerance
c) Improve health status
| REDUCE SYMPTOMS |
|
|
And
|
d) Prevent disease progression
e) Prevent and treat exacerbations
f) Reduce mortality
|
REDUCE RISK |
|
|
Chronic Management
1. COPD Assessment
Regular care reviews should be arranged for patients with COPD.
At reviews, the following should be assessed:
a. Symptoms
Symptom assessment can be performed using either
ii. Modified Medical Research Council Dyspnoea Scale (mMRC) with score of ≥2 as the cut-off for significant breathlessness.
b. Adherence to treatment and inhaler technique
c. Exacerbations in the past 12 months
i. An exacerbation is an event characterised by increased dyspnoea and/or cough and sputum that worsens in < 14 days.
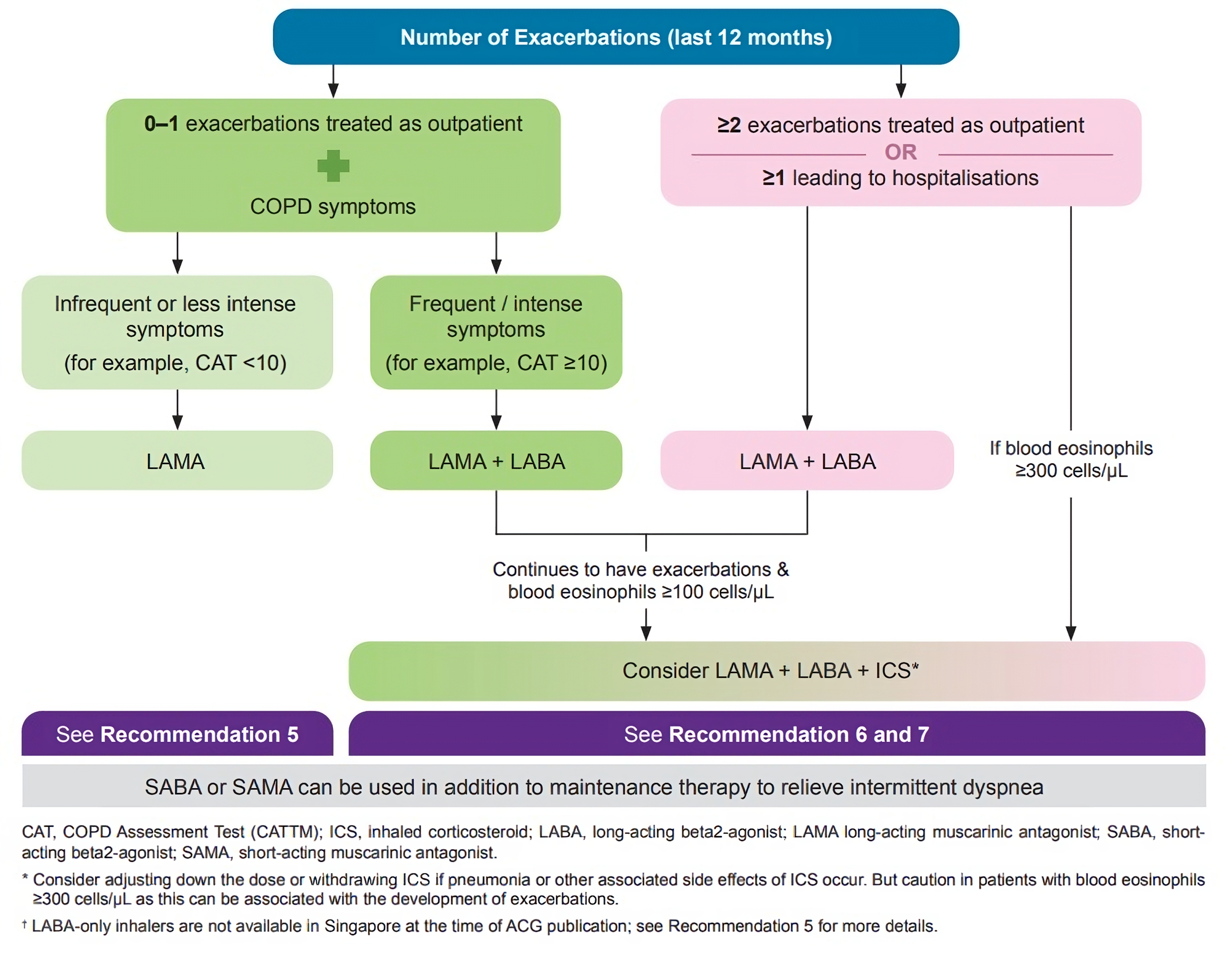
ii. Two or more exacerbations requiring antibiotics or steroids in the previous year, or one exacerbation leading to hospitalisation in the previous year, indicates increased exacerbation risk.
iii. Start bronchodilator treatment, preferably a long-acting muscarinic antagonist (LAMA), for patients with infrequent or less intense symptoms and lower risk of exacerbations.
** Submission of the CAT score is required for subsidy claims and Healthier SG payments
2.Pharmacotherapy is based on individualised symptom and assessment risk.
Examples of Whitelisted inhalers^:
|
SABA |
Salbutamol 100 mcg/dose Inhaler |
SAMA |
Ipratropium Bromide 20 mcg/dose Inhaler |
LAMA |
Umeclidinium 62.5 mcg/dose Powder inhaler (30 doses) |
LAMA/LABA |
Umeclidinium 62.5 mcg/dose + vilanterol 25 mcg/dose powder inhaler (30 doses) |
ICS/LABA
|
Salmeterol 50 mcg/dose + fluticasone propionate 500 mcg/dose powder inhaler (Seretide Accuhaler) (60 doses) |
Formoterol fumarate dihydrate 4.5 mcg/dose + budesonide 160 mcg/dose (Symbicort) Turbuhaler (120 doses) |
^Please refer to
HSG whitelist for the full list of subsidised drugs
Monitor for response to initial therapy by assessing for improvement in patient symptoms and episodes of exacerbations.
If response to therapy is appropriate, maintain the dose of effective treatment.
If response to therapy is not appropriate, check adherence, inhaler technique and possible co-morbidities.
a. Use of short- and long-acting bronchodilators
SABA or SAMA may be used as needed to relieve intermittent dyspnoea in all COPD patients. Short-acting bronchodilators alone can be considered in patients with very occasional dyspnoea. Long-acting bronchodilators are preferred as the initial maintenance therapy. Regular use of long-acting bronchodilators improves lung function, dyspnoea, health status, and reduces exacerbation rates. Long-acting muscarinic antagonists (LAMAs) are usually preferred over long-acting beta2 -agonists (LABAs), with evidence suggesting some reduction in exacerbation rates with LAMAs compared to LABAs. The
ACE patient education aid on Bronchodilator Inhalers for Chronic Obstructive Pulmonary Disease can be used to facilitate discussion with your patients on the use of bronchodilators.
b. Role of Inhaled Corticosteroids (ICS)
ICS has a limited role in COPD management.
Long-term monotherapy with ICS is NOT recommended.
Use of LABA+ICS is not encouraged in COPD. It is recommended that ICS be used as therapy additional to LABA and LAMA for select groups of patients who are either at higher risk for exacerbations or have frequent exacerbations. This combination can be given as a single or multiple inhaler therapy.
i. Initial treatment with triple therapy (LAMA + LABA + ICS)
Initiating treatment with triple therapy (LAMA + LABA + inhaled corticosteroid [ICS]) could be considered if the patient is assessed to be at a higher risk for exacerbations (for example, two or more exacerbations of COPD requiring antibiotics or steroids per year or history of hospitalisation(s) for COPD) and have blood eosinophils ≥300 cells/µL.
ii. Escalation to triple therapy (LAMA + LABA + ICS)
For patients who continue to have frequent exacerbations on LAMA + LABA therapy and have elevated blood eosinophil levels (blood eosinophils ≥100 cells/µL), addition of inhaled corticosteroid (ICS) to LAMA + LABA therapy should be considered. It has been shown to improve lung function, patient reported outcomes, and reduce exacerbations when compared to dual long-acting bronchodilator therapy.
c. Role of mucolytics
The use of mucolytics should be reserved as adjuncts to inhaled therapy.
3. Smoking cessation
Smoking cessation is a
key intervention for all COPD patients who are currently smoking. Even brief (3-minute) smoking cessation counselling is effective and such advice should be offered at every healthcare visit.
The
2 As approach provides a helpful framework to guide healthcare providers in helping COPD patients quit smoking:
i.
Ask about smoking - systematically identify all tobacco users at every visit
ii.
Act to help all tobacco users quit

4. Physical Activity
Patients should be strongly encouraged to exercise regularly and to increase their exercise levels within tolerable limits. Walking 20 to 30 minutes 3 to 4 times a week and other moderate-intensity exercises are beneficial. Adding strengthening exercises like repeated movement with weights has additional benefits. Referral to a pulmonary rehabilitation program, where available, may be considered for patients who are breathless or more symptomatic on activity and require further assessment and education on how to manage their breathlessness.
5. COPD Education*
a. COPD patients & their carers should be provided with the knowledge and skills training to enable them to self-manage their COPD well.
b. Key components of COPD education are:
i. Understanding of the disease
iii. Symptom recognition and what to do in a COPD exacerbation
v. Checking adherence to treatment plan and explore reasons for non-adherence
vi. Exercise and nutrition advice
*For PCN GPs, consider referring to PCN Nurses for additional counselling and support.
6. Preventive Care
a. Ensure that influenza, pneumococcal and COVID-19 vaccinations are up to date. Please refer to the table on Recommended Care Components below for further details on vaccinations for patients with COPD.
b. Promote recommended vaccinations as per NAIS recommendations
.
c. Offer Tdap vaccine to patients who have not received Pertussis vaccination.
d. Check smoking history regularly and advise smoking cessation if appropriate. Refer to smoking cessation clinic and offer smoking cessation medications if patient is agreeable.
e. Advise on haze precautions when appropriate.
7. Follow-up
Arrange regular follow-ups.
Recommended follow-up for patients with COPD
After an exacerbation |
Follow-up within 1 to 2 weeks or as per clinical discretion |
After starting or adjusting treatment |
Follow-up within 1 to 3 months |
All patients |
Follow-up every 12-24 weeks or more frequently as indicated |
Referrals to Respiratory Physicians
Consideration for Specialist Referral :
1. Management difficulties:
2. Symptoms disproportionate to FEV1
3. Frequent infections and infective exacerbations (e.g. more than 2 episodes in 6 months)
4. Development of new symptoms e.g. haemoptysis, or new physical signs e.g. cyanosis, peripheral oedema
5. For initiation of home oxygen therapy (i.e. long term oxygen therapy*)
*
Long term oxygen therapy (LTOT) is indicated when:
-
SaO2
<88% on room air when stable (confirmed twice over a three-week period); or
-
SaO2
=88% on room air with evidence of right heart failure or erythrocytosis.
Management of COPD exacerbations in Primary Care
Assess patients presenting with symptoms and signs of a COPD exacerbation in primary care as soon as possible to determine the severity of the exacerbation.
Patients with severe COPD exacerbation should be transferred to the emergency department as soon as possible, preferably via ambulance.
1. Signs/symptoms of an acute exacerbation:
b. Increased sputum volume
c. Increased sputum purulence (thickness or tenacity)
d. With increased cough/wheeze
2. Consider and exclude differential diagnosis of COPD exacerbations: e.g.
a. Acute coronary syndrome
e. Congestive cardiac failure
3. Administer Rescue Therapy (Example below)
Via
- Metred dose inhaler (MDI) + spacer: Salbutamol 10 puffs + Ipratropium 4 puffs via spacer
or
- Nebulized* Salbutamol (Ventolin): Ipratropium (Atrovent): Normal Saline 1: 2: 1
*Air driven nebulisation is preferred to oxygen driven, to avoid risk of increasing PaCO2.
Monitor patients closely in the clinic.
Consider oral corticosteroids.
Consider oral antibiotics when signs of bacterial infection are present.
Transfer patients with worsening condition to the emergency department by ambulance for further management.
4. If Oxygen therapy is available
If patient has SpO2 <92% and/or reduction of >3% (if baseline SpO2 is known), administer controlled Oxygen Therapy: start O2 at lowest flow that can maintain SpO2 88-92%
with minimum effective flow of oxygen.
If no pulse oximeter is available, limit supplementary O2 to 28% with mask or no more than 2L/min via nasal prongs.
5. Reassess after Rescue Therapy
Re-assess the patient after 20-30 minutes of starting bronchodilator therapy.
Refer to Emergency Department if patient has severe dyspnoea &/ indications for referral to Emergency Department.
6. Consider referral to Emergency Department:
a. Severe
signs and symptoms (e.g., sudden worsening of resting dyspnoea, high respiratory rate ≥ 24 breaths per min, reduced oxygen saturation).
b. Confusion, drowsiness.
c. Haemodynamically unstable.
d. Signs of heart or respiratory failure (e.g., cyanosis, peripheral oedema).
e. Failure to respond to initial rescue therapy.
f. Presence of serious co-morbidities (e.g., congestive heart failure or new onset arrhythmias).
g. Insufficient home support.
7. Additional factors to consider when deciding if the patient should be treated as an outpatient or referred to the Emergency Department
|
Outpatient treatment |
Consider ED referral |
Level of activity / Effort tolerance |
Good |
Poor (e.g. bedbound) |
New changes on chest radiograph |
No |
Present |
Able to cope at home |
Yes |
No
|
8. Outpatient Treatment
Patients whose condition have improved and have adequate resources to be cared for at home may be discharged home with:
a. Bronchodilator therapy:
i) SABA as needed (do not prescribe SAMA if patient is being given LAMA).
ii) Continue/start stable COPD management with regular long-acting inhaled bronchodilator
b. Oral beta-lactam antibiotic (e.g., co-amoxiclav), a macrolide or doxycycline for at least a 5-day duration, if >=2 of the following is present:
i) Increased dyspnoea
ii) increased sputum volume
iii) increased sputum purulence
A review within a week is recommended.
Recommended Care Components for COPD
Recommended Care Components |
Minimum Frequency (or more frequently if clinically indicated) |
Remarks |
Weight and BMI assessment |
Annually | Nutritional intervention should be considered in all COPD patients with BMI < 18.5kg/m2 or significant involuntary weight loss (> 10% during the last 6 months or > 5% in the past month)
|
COPD Assessment Test (CAT) score |
Annually | |
Smoking Assessment |
Annually |
Assessment on smoking habits (estimated sticks/day; zero for non-or ex-smoker) and provide smoking cessation counselling. |
Self-management education |
At diagnosis, and whenever there is a change of medication. | |
Spirometry |
At diagnosis |
Spirometry services are available at selected PCN HQs. GPs should check with their respective PCNs if spirometry is offered. |
Influenza Vaccination |
Annually or per season for:
- Patients with COPD aged 18 to 64 years; and
- All persons aged 65 years and older |
As recommended under the NAIS. |
Pneumococcal vaccination | Those who have not previously received any pneumococcal vaccine can either receive: For those who received PCV13 and/or PPSV23 but not completed the recommended vaccination series can either:
18 to 64 years of age: a) 1 dose of PCV20; or b) 1 dose of PPSV23
All persons aged 65 years and older: a) 1 dose of PCV20; or b) 1 dose of PCV13 followed by 1 dose of PPSV23 at an appropriate interval after PCV13 (and any previous PPSV23 dose)
|
For further details on dose schedule for PCV20, or PCV13 and PPSV23 based on age and medical conditions, please refer to NAIS.
|
COVID-19 Vaccination |
One initial COVID-19 dose for unvaccinated patients aged 5 years and above. #
An additional dose around one year (and not earlier than five months) after the last dose received for patients aged 6 months and above.
# Two initial doses (eight weeks apart) for unvaccinated persons aged 6 months – 4 years |
As recommended in
MOH Circular No. 80/2024 dated 25 October 2024, for all persons aged 60 years and older, medically vulnerable individuals (e.g. chronic lung conditions) and residents of aged care facilities.
|

